Effects of Common Weight Loss Surgery on the Bones of Young Individuals
According to research, weight-loss surgery frequently conducted on obese adolescents and young adults can have detrimental effects on bone health.
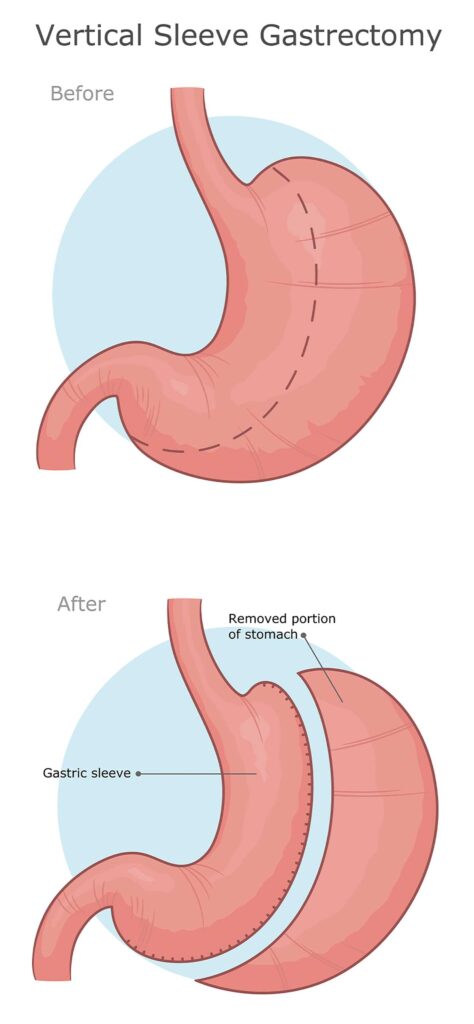
Childhood obesity rates are on the rise and surgery for weight loss is an effective means of decreasing weight and improving cardiometabolic comorbidities. This study explored the long-term effect that sleeve gastrectomy (the most popular form of surgery for weight loss) had on bone marrow fat content and bone strength among adolescents and young individuals following surgery for weight loss.
Sleeve gastrectomy involves surgically removing between 75% to 80% of the stomach in order to limit food consumption and promote weight loss. It typically creates a round stomach in the shape of a tube.
Annual estimates show an approximate increase from over 28,000 procedures performed annually in 2011 to over 122,000 procedures performed each year in 2020 – overtaking gastric bypass as the primary weight-loss solution.
Individuals between 13-24 years were recruited between 2015 and 2020 for this study, from 2015-20. Participants ranged in ages 13-24 years. Adolescents and young individuals participating were considered moderately to severely obese; young individuals had BMI of 35 or greater; obese individuals are defined as BMI of 30 or higher or greater; participants in the study reached 120% of the 95th percentile for gender and age-specific percentiles.
On this study of 54 participants, 29 were placed into a control group and 25 underwent sleeve gastrectomy surgery – 41 were female participants. Of those having surgery, at least one co-morbidity related to obesity or having a BMI greater than 40 was required; on the other hand, individuals in the control group who were obese but didn’t plan to undergo sleeve gastrectomy received exercise and diet counseling instead.
Before and 24 months post sleeve gastrectomy procedures, participants underwent blood tests, physical exams, and quantitative computed tomography (QCT) of the lumbar spine to measure volumetric bone mineral density as well as finite element analysis – an approach which assesses bone strength. QCT provides an extremely precise method for monitoring volumetric changes due to intense weight loss.
Research has demonstrated that bone marrow fat responds to nutritional changes and may act as an early biomarker of bone quality. Therefore, proton MR spectroscopy was administered to patients to measure lumbar spine bone marrow fat content.
BMI in adolescents and young adults decreased significantly two years post surgery; there was a small rise among control group. By comparison, those undergoing sleeve gastrectomy experienced significant bone marrow fat increase while strength estimates and density estimates in their lumbar spine dropped considerably.
Scientists recently conducted research that demonstrated bone strength was reduced two years following surgery for weight loss and bone marrow fat, an indicator of bone weakness, was elevated, showing surgery has an adverse impact on bone health.
Building bone mass during adolescent years is of great significance and any reductions in bone accumulation could have serious repercussions later in life and increase fracture risks for adolescents.
As bariatric surgery becomes more popular among adolescents, its effect on bone health should be highlighted to healthcare providers who will continue providing regular medical attention for these individuals.