Improving Metabolic Health in Type 2 Diabetes Through Time-Restricted Eating
Studies have revealed that following a time-restricted eating regimen limiting food consumption to within an approximate 10-hour window shows promising metabolic results among type 2 diabetes individuals.
Modern society provides its residents with endless food availability, while their circadian rhythm has been affected by irregular patterns of sleep activity and artificial lighting exposure. Individuals in Western countries tend to eat over 14 hours each day resulting in no proper nighttime fasting state.
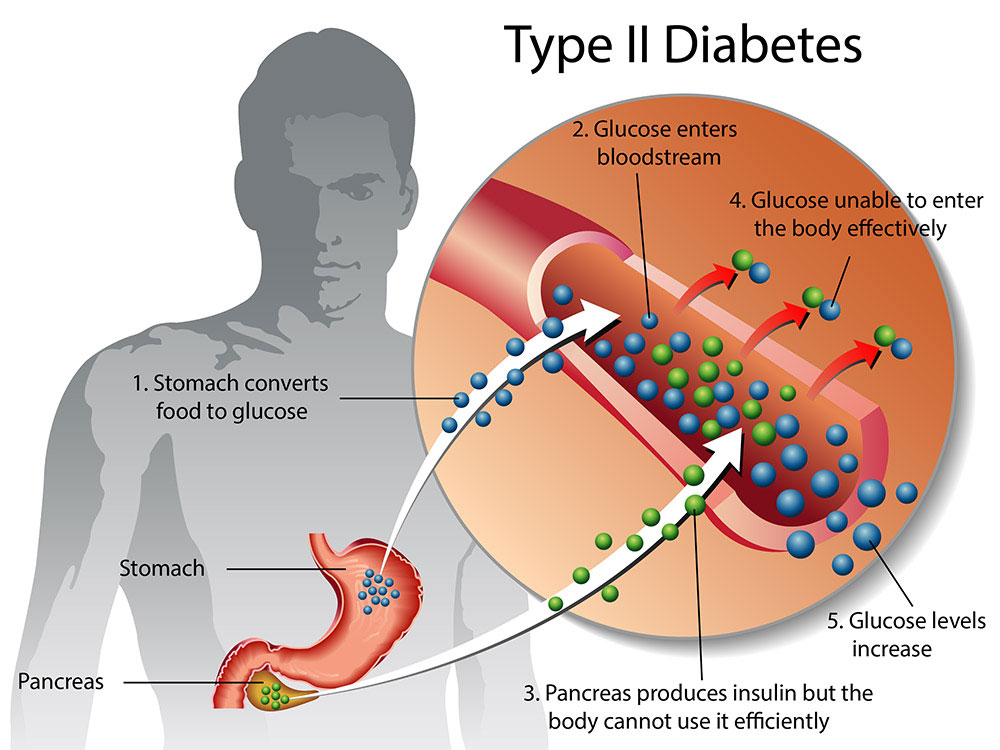
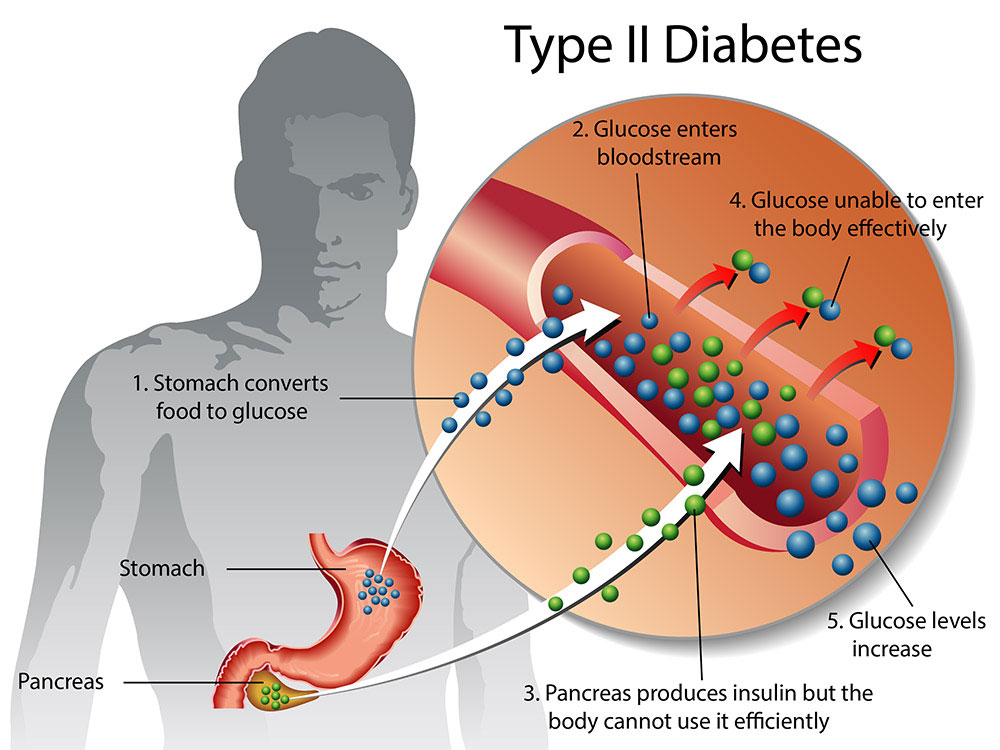
These factors all play a part in type 2 diabetes’s global prevalence and death toll; estimates from WHO show it claims more than 1.5 million victims every year.
Time-restricted eating (TRE) is a method for improving metabolic health that seeks to offset daytime eating’s harmful effects by restricting food consumption duration, restoring your daytime eating cycle, and lengthening evening and nighttime fasting periods.
Research has indicated that time-restricted eating results in positive metabolic changes for obese or overweight individuals, including increased insulin sensitivity, reduced blood sugar levels, and enhanced fat burning; but its exact effects remain unknown. Although promising, such studies often use extremely short eating window (6-8 hours) and highly controlled settings which make such regimens hard to implement into everyday life.
Time-restricted eating may result in unexpected weight loss that appears to improve metabolic health; however, improvements have also been observed without weight loss; this suggests other mechanisms are at work when time-restricted eating impacts metabolism.
Researchers suggest that metabolic health impaired people often exhibit altered metabolic process rhythm changes when compared with healthy and lean individuals, suggesting a disturbed eating-fasting cycle could contribute to these rhythm changes. They further propose restricting food consumption to only daytime hours while lengthening nighttime fast times could improve metabolic health.
This study included 14 adults between 50 and 75 years of age who had type 2 diabetes with BMI of 25 kg/m2. It consisted of two intervention periods of three weeks each: time-restricted eating period and control period, each separated by a washout duration of at least 4 weeks.
At the start of each intervention, body weight was assessed and individuals were provided with a glucose monitoring device which continuously measured blood sugar levels every 15 minutes. They were encouraged to maintain their usual physical activity and sleeping patterns and maintain stable weight by keeping a sleep and food diary throughout both interventions; this ensured their diet would be consistent in terms of both quality and quantity during subsequent periods.
Individuals during the time-restricted eating period were required to consume a normal diet within 10 hours per day and no later than 6 PM, and finish eating no later than this time frame. They were allowed to break this schedule up with black coffee, plain tea or water consumption throughout the day or moderate consumption of zero-calorie soft drinks during evening timeframe. Participants only needed to spread out their normal food consumption over 14 hours during control period.
Time-restricted eating was conducted over an average period of 9.1 hours compared to 13.4 in control; sleep duration ranged between 8.1 hours and 8.0 hours respectively in both cases. Body mass at baseline for time-restricted and control participants was similar, yet small but significant weight loss resulted from time-restricted eating but not control.
Time-restricted eating was found to lower 24-hour glucose levels significantly, due primarily to decreased nighttime blood sugar. Average normal blood glucose range duration increased from 12.2 hours during the control phase to 15.1 hours on average with time-restricted eating group experiencing consistently lower fasting morning glucose levels than the control diet group due possibly to changes in nighttime blood sugar regulation.
Reducing time-restricted eating did not significantly extend low blood sugar duration and no serious adverse reactions were reported, suggesting that an eating frame of about 10 hours is an effective and safe lifestyle intervention for type 2 diabetes individuals.
Liver glycogen levels were assessed during each intervention following either 10- or 14-hour overnight fasts; measurements were also taken at the beginning and end of each study period following 11-hour fasts to compare time-restricted eating to controls; there was no significant difference in liver glycogen between time-restricted eating and controls, and liver fat analysis revealed no disparate composition or quantity differences among them.
Contrary to a prior study on time-restricted eating, this one did not find that time-restricted eating had any impact on insulin sensitivity. That earlier research had used much shorter 6-hour food consumption frames with the last meal being eaten at 3 PM – leading to longer fasting periods which might prove more effective, yet impractical for most type 2 diabetes individuals living modern lifestyles.
Researchers found that following a three-week daytime 10-hour time-restricted eating regime reduces glucose levels and extended normal blood sugar range duration in type 2 diabetes individuals in comparison with spreading food consumption across 14 hours or more per day.